Scientific Calendar July 2020
Pyelonephritis
Pyelonephritis, technically, refers to ...
Inflammation of the kidney
Inflammation of the ureter
Inflammation of the renal pelvis
Inflammation of the urethra
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Laboratory results
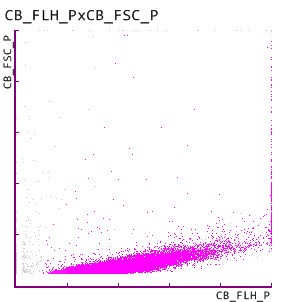
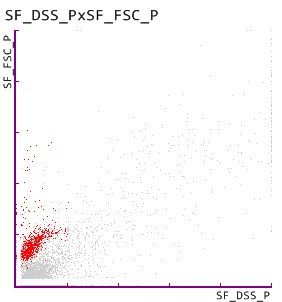
1. Bacterial cell count on the UF-5000
The detection of ≥ 105 CFU/mL and the suspicion of gram-negative bacteria, indicated by the ‘Gram negative?’ BACT-Info flag, reveals the presence of a bacteriuria by gram-negative Escherichia coli, as confirmed by urine culture.
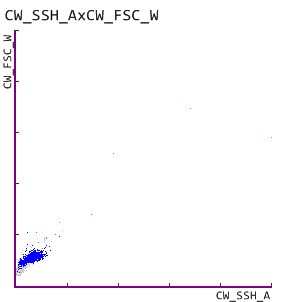
2. White blood cell (WBC) count on the UF-5000
The detection of WBC reveals pyuria and indicates the presence of an infectious condition.
3. Renal tubular epithelial cells (RTEC) on the UF-5000
The UF-5000 detected renal tubular epithelial cells (RTEC), which usually cover the renal tubules from the proximal tubule via the loop of Henle to the distal tubule. Considering a recent publication by Oyaert et al. that reported a clinical utility of the RTEC count in diagnosing upper urinary tract infection, the detection of RTEC supports the diagnosis of a pyelonephritis.
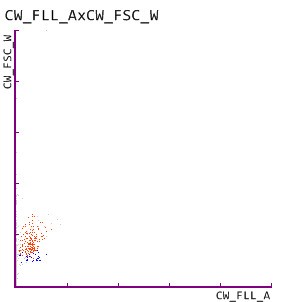
4. Dysmorphic RBC on the UF-5000
The UF-5000 further confirmed a persistent haematuria by the detection of dysmorphic RBC, which are known indicators of glomerular damage, and the findings are in line with the patient history.
References
Birch DF, Fairley KF (1979): Haematuria: Glomerular or Non-Glomerular? Lancet 2(8147):845–846.
Birch DF, Fairley KF, Whitworth JA, Forbes I, Fairley JK, Cheshire GR, Ryan GB (1983): Urinary Erythrocyte Morphology in the Diagnosis of Glomerular Hematuria. Clin Nephrol 20(2):78–84.
Flores-Mireles AL, Walker JN, Caparon M and Hultgren SJ (2015): Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol 13(5):269–284.
Lane DR and Takhar SS (2011): Diagnosis and Management of Urinary Tract Infection and Pyelonephritis. Emerg Med Clin North Am 29(3):539–552.
De Rosa R, Grosso S, Lorenzi S, Bruschetta G, Camporese A (2018): Evaluation of the new Sysmex UF-5000 fluorescence flow cytometry analyser for ruling out bacterial urinary tract infection and for prediction of Gram-negative bacteria in urine cultures. Clinica Chimica Acta 484:171–178.
Oyaert M, Speeckaert M, Boelens J, Delanghe JR (2020): Renal tubular epithelial cells add value in the diagnosis of upper urinary tract pathology. Clin Chem Lab Med 58(4):597–604.
Scientific background
A pyelonephritis is a complicated urinary tract infection characterised by bacterial infiltration of the renal tissue and renal pelvis that can be either acute or chronic. The common pathogenic course of an acute pyelonephritis is often an ascending extraluminal bacterial infection by microbial contamination of the periurethral zone and subsequent colonisation towards the bladder and further migration into the renal pelvis. Pyelonephritis in male or pregnant individuals, in the context of anatomical malformation or underlying renal disorders or infection-promoting concomitant diseases (e.g. diabetes mellitus) is considered a complicated pyelonephritis.
Clinically, a pyelonephritis is a severe disease with high fever, flank pain, an intense feeling of sickness and the presence of bacteriuria. The pathogen spectrum of a pyelonephritis is dominated by Escherichia coli and enterococci, followed by Proteus mirabilis, Klebsiella pneumoniae and staphylococci.
An acute pyelonephritis can turn into a chronic pyelonephritis by formation of small abscesses due to improper treatment or by vesico-ureteral reflux – the reflux of urine from the lower into the upper urinary tract. The enrichment of bacteria within the regurgitant urine can cause recurrent infection and scarred pyelonephritis. Although the chronic pyelonephritis can remain asymptomatic for a long time, it can cause end-stage renal failure and compulsory dialysis.
Complications of the acute pyelonephritis include urosepsis, septic shock, damages of the renal parenchyma by scarred healing or emphysematous pyelonephritis in the context of diabetes mellitus.
The diagnosis of acute pyelonephritis is primarily based on fever, flank pain and pyuria. Laboratory diagnostics include CBC+DIFF, ESR, CRP and urinalysis. Urinalysis usually reveals pyuria, bacteriuria, mild proteinuria, micro- or macro-haematuria and leucocyte casts. In addition, imaging studies support the differential diagnosis and the detection of complications.