Scientific calendar July 2022
Thrombotic events in patients with afibrinogenaemia
In which clinical conditions may patients with afibrinogenaemia develop a thromboembolic event?
In the presence of a concomitant acquired or inherited thrombophilia disorder.
Under treatment with fresh frozen plasma or cryoprecipitates.
Afibrinogenaemia as such is a clinical condition that poses a thrombotic risk.
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific background
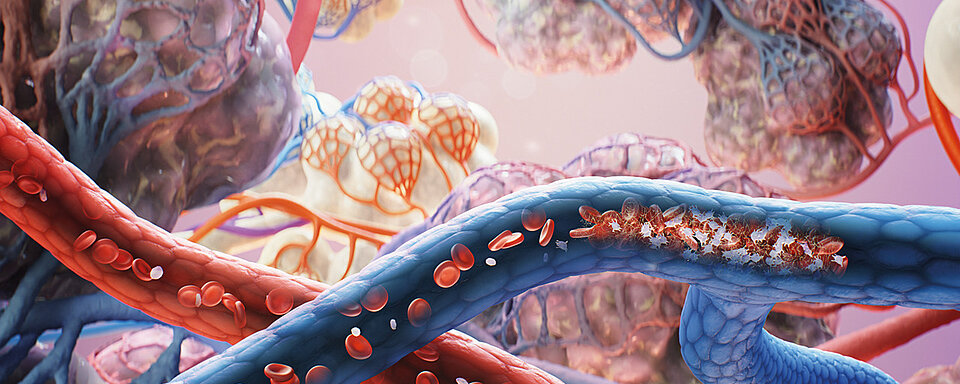
Afibrinogenaemia is the complete absence of fibrinogen and characterised by bleeding that typically occurs in the neonatal period with umbilical cord haemorrhages. Other haemorrhages may occur in the skin, soft tissues, muscles, joints, gastrointestinal tract, or genitourinary tract. Intracranial haemorrhages occur less frequently but can be recurrent and are often fatal. [1, 2] The tendency to bleed varies widely, ranging from very few to several episodes a year. In individuals with afibrinogenaemia, clot-based coagulation tests are indeterminately prolonged and fibrinogen activity and antigen are undetectable. [3, 4]
| Laboratory parameter | Result of afibrinogenaemic patients |
| Prothrombin time (PT) | No coagulation |
| Activated partial thromboplastin time (APTT) | No coagulation |
| Thrombin time | No coagulation |
| Fibrinogen activity | Undetectable |
| Fibrinogen antigen | Undetectable |
Table 1 Laboratory parameters in patients with afibrinogenaemia
Patients with afibrinogenaemia have a significantly increased risk of thromboembolic events in addition to an increased risk of bleeding. These events occur already at a young age and are often recurrent arterial or venous thromboses. In quite a few cases, the clot migrates into the pulmonary vessels, leading to the obstruction or stenosis of a pulmonary or bronchial artery. Less often seen thrombotic events include mixed forms of arterial and venous thrombosis. [4, 5, 6]
The increased thrombotic risk in fibrinogen-abstinent individuals can be explained primarily by the antithrombotic effect of fibrin, in addition to the presence of common risk factors for thrombosis, such as smoking, high blood pressure, obesity and the use of oral contraceptives [7, 8, 9]. Fibrin reduces the activation of prothrombin and also binds thrombin circulating in the blood. [10, 11] In the absence of fibrin, free thrombin remains available for platelet activation and, among other things, various growth factors are released which induce proliferation of vascular smooth muscle cells. [12, 13] Soluble fibrinogen is also able to inhibit platelet adhesion. In patients with afibrinogenaemia, the antithrombotic function of both fibrin (also called antithrombin I) and fibrinogen is absent. Furthermore, thrombus formation is maintained by other adhesive proteins, such as fibronectin or von Willebrand factor. The resulting thrombi are usually loosely packed, therefore unstable and prone to mobilisation. [13]
Another risk of thromboembolic events in individuals with afibrinogenaemia is the concomitant presence of acquired or inherited thrombophilia disorders. Individuals with congenital antithrombin III deficiency have a significantly increased risk of spontaneous severe arterial occlusion, such as acute coronary syndrome and stroke, venous thrombosis, and pulmonary embolism. [14] Similar cases have also been reported in association with concomitant protein C deficiency. [15, 16] Acquired risk factors include underlying infections or malignancy.
Fibrinogen substitution poses an additional risk to patients with afibrinogenaemia. Fresh frozen plasma (FFP) and cryoprecipitates contain fibrinogen and large amounts of other proteins such as fibronectin, VWF and factor VIII, providing a procoagulant environment. FFP also bears other transfusion-related risks such as transfusion-related acute lung injury or the undesirable infusion of microorganisms.
Fibrinogen concentrate (FC) substitution is the replacement therapy of choice in patients with afibrinogenaemia, as this has fewer risks of adverse side effects while having a higher treatment efficacy. [17] It has also been demonstrated that administration of FC can effectively reduce platelet adhesion and platelet aggregation even at low fibrinogen concentrations. [13, 18] Women with afibrinogenaemia have a higher probability of a successful pregnancy if they are treated early on with FC or cryoprecipitates and the amount substituted is adjusted to the fibrinogen requirement during pregnancy.
The management of patients with afibrinogenaemia can be challenging because in addition to the prevention and treatment of bleeding, the prevention and, in the worst case, treatment of thrombosis must be delivered in parallel. The treatment of thrombotic events includes the administration of anticoagulants, aggregation inhibitors and fibrinolytics. [19, 20] The treatment of bleeding episodes should ideally be performed with FC, individually adapted to age, weight and current circumstances (e.g. pregnancy), and include therapy monitoring by means of a fibrinogen activity test. [21, 22]
References
[1] de Moerloose P, Neerman-Arbuz M. (2009): Congenital fibrinogen disorders. Semin Thromb Hemost; 35: 356–366.
[2] Acharya SS, DiMichel DM. (2008): Rare inherited disorders of fibrinogen. Haemophilia; 14: 1151–1158.
[3] Neerman-Arbez M, et al. (2016): Laboratory and Genetic Investigation of Mutations Accounting for Congenital Fibrinogen Disorders. Semin Thromb Hemost; 42(04): 356–365.
[4] Alessandro Casini, Marguerite Neerman-Arbez, Philippe de Moerloose. (2021): Heterogeneity of congenital afibrinogenemia, from epidemiology to clinical consequences and management. Blood Reviews; Volume 48, 100793.
[5] Lak M, et al. (1999): Bleeding and thrombosis in 55 patients with inherited afibrinogenaemia. Br J Haematol; 107: 204–206.
[6] Bornikova L, et al. (2011): Fibrinogen replacement therapy for congenital fibrinogen deficiency. Journal of Thrombosis and Haemostasis; 9: 1687–1704.
[7] Abdollahi M, Cushman M, Rosendaal FR. (2003): Obesity: risk of venous thrombosis and the interaction with coagulation factor levels and oral contraceptive use. Thromb Haemost; 89(3): 493–498.
[8] Newby DE, et al. (1999): Endothelial dysfunction, impaired endogenous fibrinolysis, and cigarette smoking: a mechanism for arterial thrombosis and myocardial infarction. Circulation; 99: 1411–1415.
[9] Leone A. (2007): Smoking, haemostatic factors, and cardiovascular risk. Curr Pharm Des; 13(16): 1661–1667.
[10] Mosesson MW. (2003): Antithrombin I. Inhibition of thrombin generation in plasma by fibrin formation. Thromb Haemost; 89(1): 9–12.
[11] de Bosch NB, Mosesson MW, Ruiz-Saez A, Echenagucia M, Rodriguez-Lemoin A. (2002): Inhibition of thrombin generation in plasma by fibrin formation (Antithrombin I). Thromb Haemost; 88(2): 253–258.
[12] Dupuy E, et al. (2001): Embolized ischemic lesions of toes in an afibrinogenemic patient: possible relevance to in vivo circulating thrombin. Thromb Res; 102(3): 211–219.
[13] Korte W, Feldges A. (1994): Increased prothrombin activation in a patient with congenital afibrinogenemia is reversible by fibrinogen substitution. Clin Investig; 72(5): 396–398.
[14] Le Quellec S, Desjonqueres A, Rugeri L, et al. ( 2018): Combined life-threatening thromboses and hemorrhages in a patient with afibrinogenemia and antithrombin deficiency. Thrombosis J; 16, 6.
[15] De Mattia D, Regina G, Giordano P, Del Vecchio GC, Altomare M, Schettini F. (1993): Association of Congenital Afibrinogenemia and K-Dependent Protein C Deficiency—A Case Report. Angiology; 44(9): 745–749.
[16] Hanano M, Takahashi H, Itoh M, Shibata A. (1992): Coexistence of congenital afibrinogenemia and protein C deficiency in a patient. Am J Hematol; 41(1): 57–60.
[17] Casini A, de Moerloose P. (2020): Fibrinogen concentrates in hereditary fibrinogen disorders: Past, present and future. Haemophilia; 26(1): 25–32.
[18] Reininger AJ, et al. (1995): Effect of fibrinogen substitution in afibrinogenemia on hemorheology and platelet function. Thromb Haemost; 74(3): 853–858.
[19] Sartori MT, et al. (2015): Thrombosis of abdominal aorta in congenital afibrinogenemia: case report and review of literature. Haemophilia; 21(1): 88–94.
[20] Castaman G, et al. (2009): Severe spontaneous arterial thrombotic manifestations in patients with inherited hypo- and afibrinogenemia. Haemophilia; 15(2): 533–537.
[21] Khayat CD, et al. (2020): Pharmacology, Efficacy and Safety of a Triple-Secured Fibrinogen Concentrate in Children Less than or Equal to 12 Years with Afibrinogenaemia. Thromb Haemost; 120(6): 957–967.
[22] Bellon A, et al. (2020): Population pharmacokinetics of a triple-secured fibrinogen concentrate administered to afibrinogenaemic patients: Observed age- and body weight-related differences and consequences for dose adjustment in children. Br J Clin Pharmacol; 86: 329–337.