In search of better biomarkers to support sepsis diagnosis
In this interview, Dr Eloisa Urrechaga, a senior expert in clinical chemistry at Biocruces Bizkaia Health Research Institute, Barakaldo in Spain, shares her passion for pushing boundaries of laboratory medicine for better diagnosis and management of sepsis.
When did you become interested in using cell functionality and activation white blood cell parameters in connection with the diagnosis and management of sepsis?
That was when I started working with Sysmex XN-Series analysers. Previously, I had been working with advanced RBC parameters and RET-He, but when I moved to the new core lab, I started to familiarise myself with the WBC scattergrams, a system which was radically different from my experience with other analysers.
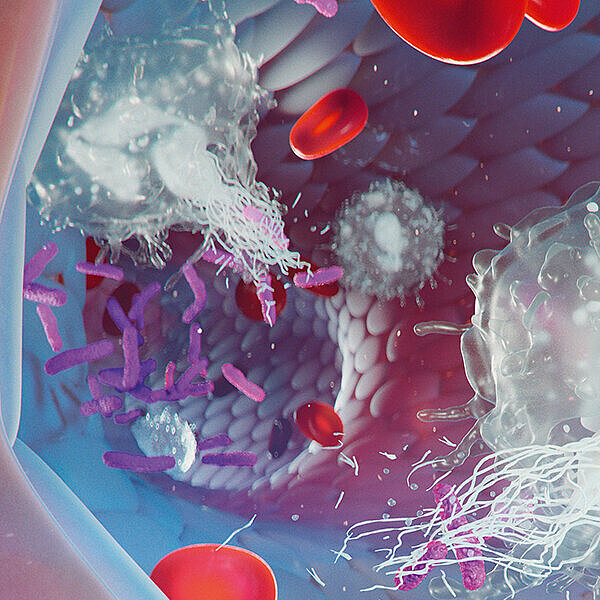
The concept of WBC activation parameters was also new for me, so I began studying the technical basis and tried to verify the potential value based on our daily workload. I selected sepsis because it is a highly lethal disease – a medical emergency involving a dysregulated systemic immune response to an infection, so I was expecting this to have a clear effect on the WBC activation parameters.
Fast and appropriate therapy is a cornerstone when it comes to sepsis. However, the discrimination of sepsis from non-infectious causes of inflammation may be difficult, and biomarkers have been suggested to aid physicians in this decision. Procalcitonin (PCT) is currently the most frequently recommended biomarker for this purpose. But when we retrospectively evaluated the medical records of our septic patients, we found that 45% of them had low PCT values at admission. So, we wanted to evaluate the potential contribution of white blood cell activation parameters to improve the detection of patients at risk of developing sepsis.

What made you think that advanced laboratory parameters coming from routine haematology analysers could significantly contribute to managing sepsis, one of the key problems of modern medicine?
The ‘golden hour’ is the term often used in emergency care to suggest that an injured or sick person must receive definitive treatment within the first 60 minutes from the onset of symptoms. Early diagnosis and rapid intervention are essential to improve outcomes. But correctly diagnosing by clinical examination, biochemical markers and microbiological blood cultures is both costly and time-consuming. A quick initial indication would be beneficial since this can point out the appropriate diagnostic tests while avoiding unnecessary follow-up tests, and help start treatment faster, which is essential in septic patients.
The CBC is one of the most frequently ordered laboratory tests by physicians. It is inexpensive and fast, obtainable 24/7 in hospitals of all levels, and results are often available within an hour. Over the past few decades, haematology analysers have undergone rapid development due to the technological progress. This becomes evident not only in their full automation and better performance, but also in the increased number of reported parameters.
WBC activation parameters provide quantitative information on the morphological and functional characteristics of white blood cells (neutrophils, monocytes, and lymphocytes). Their morphological characteristics can be accurately measured, and a more detailed study of these cells and their morphological variations in response to stimuli, such as infections, can offer valuable information on the state of activation and functional activity.
The clinical application of WBC activation parameters offers several advantages. These parameters are generated during a CBC, without additional costs or sample needs. The numerical data of these parameters are more objective and accurate than manual differential counts because thousands of white blood cells are automatically evaluated. And since the CBC is routinely requested by physicians as part of the management of patients with sepsis anyway, the WBC activation parameters could be used as an additional marker at a lower cost than other laboratory tests.
We wanted to evaluate the potential contribution of white blood cell activation parameters to improve the detection of patients at risk of developing sepsis.
What have been your main research results in this field so far, and do you see some promising biomarkers, or scores based on biomarkers, that could already distinguish septic from non-septic patients?
Some of WBC activation parameters are still research parameters and cannot be reported to clinicians. On the other hand, scoring systems are routinely used by the clinicians to aid in diagnosis and decision-making. Our objective was to develop predictive models and clinical prediction rules based on WBC activation parameter values that allow sepsis to be detected early with a good diagnostic performance, and to that end we composed a score (NEMO, neutrophils and monocytes), a risk score for sepsis.
The NEMO score includes WBC activation parameter values for neutrophils and monocytes characterizing the early innate immune response. Activation of this first line of defence occurs within a few minutes of the stimulus. As such, they are ideal biomarkers for an early detection of the disease and provide real-time information concerning the morphological and functional changes in white blood cells. The most relevant parameters (NEUT-RI and MONO-X) were selected to be included in the NEMO score to stratify the risk of suffering from sepsis [1]. According to their individual score value, the NEMO score classifies patients into three groups based on their probability of suffering from sepsis: 0–3 (low probability), 4–6 (medium probability) and ≥ 7 (high probability). It was found that 94.1% of these patients were correctly categorized as to their risk of suffering from sepsis. Since the NEMO score also discriminates patients with a low risk of suffering from sepsis (0–3), its use may lead to savings in terms of unnecessary antibiograms and treatments.
How do you see the general role of the central laboratory in the management of sepsis?
When seeking to promote the value of laboratory medicine we make use of what has become known as the ‘70% claim’. In sepsis, the rapid initiation of treatment reduces mortality, so the question is how laboratory medicine could efficiently contribute to achieving this – based on our data, clinicians can decide with confidence and consequently act faster. Biomarkers can be applied to diagnosis, prognosis, and therapy monitoring. FDA-approved tests are procalcitonin (may accurately differentiate sepsis from SIRS), and lactate (a useful marker for organ dysfunction, so it presents a prognostic value). Other biomarkers, such as C-reactive protein (CRP), or interleukin 6 (IL-6) have been proposed to diagnose sepsis or to predict mortality, but they currently lack sufficient sensitivity and specificity to be considered for stand-alone testing. Haematological parameters may alert clinicians to the presence of an underlying infection. Routine laboratory parameters include WBC, absolute neutrophil count, and immature granulocytes.
The second essential contribution that laboratory medicine could provide in sepsis-related diagnostics encompasses staging, prognostication, and therapeutic monitoring. Despite remarkable efforts made over the past decade to identify reliable biomarkers that may allow a timely and accurate diagnosis of sepsis, the identification and prognostication is still challenging. The biochemical parameters that have been proposed so far are characterized by several limitations, including an insufficient diagnostic performance, high cost, and a prolonged turnaround time, which would make them unsuitable for an urgent management of patients. Therefore, the use of innovative, easily accessible, and virtually inexpensive parameters represents an appealing perspective for improving the clinical outcome in septic patients. Ultimately, the goal is to improve patient care through early detection supported by rapid-response laboratory confirmation and immediate treatment.
Did you implement already some of the new findings in your hospital setting, or investigated the WBC cell functionality parameters recently during the COVID-19 pandemic?
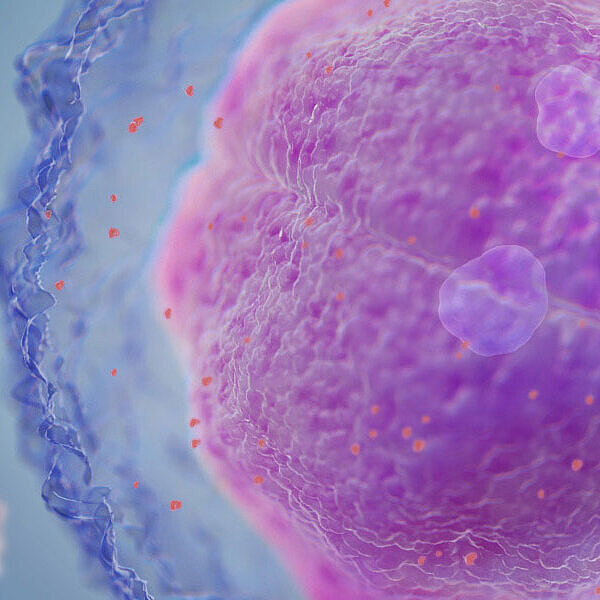
Before the pandemic outbreak in 2020 we started a multicentric project in collaboration with the pneumology department on the value of WBC activation parameters in evaluating the aetiology of community-acquired pneumonia. After the outbreak, most of our patients suffered from COVID-19. We participated in the Spanish BIOCOVID study, in which 35 laboratories were involved. The pathology of severe COVID-19 is the result of the dysregulated immune response with the attenuation of the adaptive immune system. This disbalance in immune response may be one of the features of the disease that is detectable by a laboratory. The cytokine storm is responsible for the progression and severity of the disease.
Although it is known that changes in haematologic parameters can be detected even in the early phase of infection, verifying the WBC differentials of those patients gave me a surprise since there seemed to be a recurring pattern of neutrophilia and lymphopenia despite the viral aetiology. Moreover, the presence of reactive lymphocytes (RE-LYMP) was a prominent feature, which is in clear contrast to what we see in other infections. In my opinion, the distribution of cells in WDF scattergram is highly suggestive of COVID-19 in contrast to bacterial and other viral infections.
We hypothesized that patients with infection or fever could be divided into distinct groups based on the aetiology of the infection by collectively evaluating the CBC and WBC activation parameter data. The mathematical model divided the study group into two distinctive clusters and was capable to identify 144 out of 153 COVID-19 patients (94.1%) in the validation group. More interesting and clinically relevant is that in severe cases the few lymphocytes are reactive and the proportion of activated lymphocytes clearly elevated. Cytometric analysis demonstrated that CD4+ and CD8+ T cells are substantially reduced but with hyperactive status in the peripheral blood. Using XN analysers, the reactive lymphocytes (RE-LYMP) can be quantified. The RE-LYMP and AS-LYMP parameters are part of the ‘Extended Inflammation Parameters’ and can provide quantitative information on the inflammatory reaction of the patient’s immune system. We examined the white blood cell differential and extended inflammation parameter data of the patients infected with SARS-CoV-2 and other infections of different aetiologies when admitted to the Emergency Room. To this end, a two-step algorithm with two conditions – NLR > 3.3 and RE-LYMP > 0.6% – was selected, and 153 out of 160 COVID-19 patients were correctly identified (95.6%)[2].
Dr Urrechaga, thank you very much for this exciting insight into the sepsis topic and your related research work.
References
Reference list
[1] URRECHAGA E et al. (2018): Role of leucocytes cell population data in the early detection of sepsis. J Clin Pathol. 71(3): 259-266.
[2] URRECHAGA E et al. (2021): Leukocyte differential and reactive lymphocyte counts from Sysmex XN analyzer in the evaluation of SARS-CoV-2 infection. Scand J Clin Lab Invest. 81(5): 394-400.